In a world where digital transformation is reshaping every facet of healthcare, teleophthalmology stands out as a beacon of hope for millions suffering from preventable vision loss. As the global burden of eye disease continues to rise—particularly in low-resource settings—teleophthalmology offers a revolutionary approach to diagnosing, managing, 青光眼 and even preventing ocular conditions remotely. It is not merely a technological innovation; it is a paradigm shift in how eye care is delivered, democratizing access and redefining possibilities.
The urgency of this transformation cannot be overstated. According to the World Health Organization, over 2. 2 billion people globally suffer from visual impairment or blindness, and nearly half of these cases could have been prevented or treated with timely intervention. Yet, in many parts of the world, especially rural and underserved regions, access to ophthalmologists and specialized eye care remains a distant dream. Long travel distances, high costs, and limited infrastructure create insurmountable barriers for those most in need. Teleophthalmology breaks down these barriers by bringing expert care to the patient—no matter where they are.
At its core, teleophthalmology leverages digital communication tools to facilitate remote eye examinations, consultations, and follow-ups. High-resolution imaging devices capture detailed photographs of the retina, cornea, and other ocular structures, which are then transmitted securely to specialists for evaluation. This asynchronous model—often referred to as “store-and-forward”—allows for efficient triage and diagnosis without requiring both patient and provider to be present simultaneously. In more advanced setups, real-time video consultations enable interactive assessments, particularly useful for complex cases or surgical planning.
One of the most impactful applications of teleophthalmology is in diabetic retinopathy screening. Diabetes affects hundreds of millions worldwide, and diabetic retinopathy is a leading cause of blindness among working-age adults. Regular screening is essential, yet many patients miss out due to logistical challenges. Teleophthalmology programs have successfully integrated retinal imaging into primary care clinics, allowing non-specialist staff to capture images that are later reviewed by ophthalmologists. This model has dramatically increased screening rates and early detection, leading to timely treatment and preserved vision.
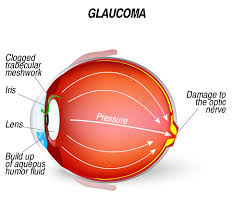
Glaucoma, age-related macular degeneration (AMD), and pediatric eye conditions also benefit from teleophthalmology. For glaucoma, remote monitoring of intraocular pressure and optic nerve imaging helps track disease progression and adjust treatment plans. In AMD, teleophthalmology facilitates early identification of wet versus dry forms, guiding appropriate interventions. Pediatric patients, often underserved due to the scarcity of pediatric ophthalmologists, can now receive expert evaluations through teleconsultations, ensuring timely care during critical developmental windows.
The COVID-19 pandemic accelerated the adoption of teleophthalmology, highlighting its value not just in remote areas but also in urban centers where in-person visits became risky or impractical. Clinics rapidly adapted by deploying secure platforms for virtual visits, enabling continuity of care while minimizing exposure. This shift also prompted regulatory bodies to revisit telemedicine policies, paving the way for broader implementation and reimbursement models that support sustainable growth.
Despite its promise, teleophthalmology is not without challenges. Technical limitations, such as poor internet connectivity and lack of standardized imaging equipment, can hinder effectiveness. Data privacy and cybersecurity are paramount concerns, especially when transmitting sensitive medical information across borders. Moreover, training non-specialist personnel to capture high-quality images and interpret basic findings requires ongoing investment and oversight.
Cultural and linguistic barriers also play a role. In some communities, patients may be hesitant to trust remote consultations or may struggle to communicate symptoms effectively. Building trust through community engagement and culturally sensitive care models is essential for long-term success. Additionally, integrating teleophthalmology into existing healthcare systems requires coordination across multiple stakeholders—primary care providers, specialists, policymakers, and technology developers.
Innovative solutions are emerging to address these hurdles. Mobile eye clinics equipped with satellite connectivity and portable imaging devices are reaching remote villages, capturing data that can be analyzed by urban specialists. Artificial intelligence is being harnessed to pre-screen images, flagging abnormalities and prioritizing cases for review. These AI algorithms, trained on vast datasets, can detect conditions like diabetic retinopathy and glaucoma with remarkable accuracy, augmenting human expertise and accelerating diagnosis.
Public-private partnerships are also playing a pivotal role. Governments, NGOs, and tech companies are collaborating to build scalable teleophthalmology networks, often integrating them into broader telehealth initiatives. These partnerships bring together funding, infrastructure, and expertise, creating robust ecosystems that can adapt to local needs. In India, for example, the Aravind Eye Care System has pioneered teleophthalmology outreach, screening millions and delivering care to those who would otherwise go untreated.
Education and awareness are critical components of teleophthalmology’s success. Patients must understand the importance of regular eye exams and feel empowered to seek care—even if it’s virtual. Healthcare workers need training not only in technical skills but also in patient communication and ethical considerations. Medical schools and continuing education programs are beginning to incorporate telemedicine modules, preparing the next generation of providers for a digitally connected world.
Looking ahead, the future of teleophthalmology is bright and expansive. As technology becomes more affordable and accessible, even the most remote communities can benefit from high-quality eye care. Integration with wearable devices, such as smart contact lenses and ocular sensors, may enable continuous monitoring of eye health, alerting providers to changes in real time. Virtual reality and augmented reality could enhance remote surgical training and patient education, making complex concepts more tangible.
Ultimately, teleophthalmology is more than a tool—it is a movement toward equity in healthcare. It embodies the principle that geography should not determine destiny, especially when it comes to something as fundamental as vision. By bridging the gap between patients and providers, urban centers and rural outposts, rich and poor, teleophthalmology is rewriting the narrative of global eye care.
In a world where sight can mean the difference between opportunity and isolation, teleophthalmology offers a lifeline. It brings hope to the farmer in a remote village, the child in an underserved school, the elderly woman unable to travel. It reminds us that innovation, when guided by compassion and purpose, can illuminate even the darkest corners of the world—one eye at a time.